
John Cassim
The interconnectedness of Antimicrobial Resistance (AMR) and HIV underscores the urgent need for Zimbabwe to fully adopt a One Health approach, recognizing the inseparable link between human health and the environment. This holistic perspective is crucial for safeguarding the effectiveness of HIV treatment.
Consequently, there’s a strong call for Zimbabwe to empower the National Aids Council (NAC) to spearhead the strategic response to the growing HIV drug resistance (HIVDR) crisis, estimated at a concerning 45%. This high level of resistance poses a significant threat, especially considering the country’s commendable 90% viral suppression rate under the 95-95-95 targets.
Several factors contribute to HIV drug resistance, with the misuse of antibiotics in treating diseases affecting both humans and animals being a primary concern. This inappropriate use can foster the development of drug-resistant microbes that can then impact individuals with HIV.
In Zimbabwe, less than 10% of the general population has Non-Nucleoside Reverse Transcriptase Inhibitors – Pretreatment Drug Resistance (NNRTI PDR). This pretreatment resistance occurs when individuals are infected with an HIV strain already resistant to certain medications, significantly complicating initial treatment. Alarmingly, NNRTI resistance affects at least 94% of youths, highlighting a critical challenge for the future of HIV care in the country. Furthermore, the increasing reliance on more expensive and complex third-line HIV treatment, which saw a substantial increase from 36 to 533 cases between 2018 and 2023, further underscores the growing problem of drug resistance.
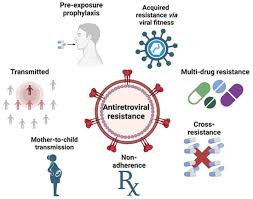
Dr. Tinashe Hodobo, a member of the One Health Secretariat, emphasized the severity of the situation during a recent NAC media workshop in Chinhoyi: “When the immune system of someone with HIV is already compromised, developing resistance makes the situation much worse. HIV combined with AMR presents a far greater challenge than either alone.” He further stressed the importance of adhering strictly to prescribed drug regimens and following professional medical guidance, including the use of laboratory data, for improved patient care and treatment outcomes.
Dr. Hodobo also highlighted the significant danger of ARV and antibiotic misuse in animals, which can contribute to the development of drug resistance in humans. “While unconfirmed rumors suggest the use of ARVs in chicken in Zimbabwe, documented cases exist in countries like Tanzania and Zambia due to inadequate regulations, monitoring, and public awareness,” he noted. “If this is happening, the implications are significant for individuals relying on these essential medicines, potentially consuming poultry with sub-therapeutic drug levels. This is a serious issue requiring thorough investigation.”
In response to this growing threat, the Zimbabwean government developed a comprehensive One Health strategy, the One Health – Antimicrobial Resistance National Action Plan 2024-2028, which was launched a few months ago.
The One Health Strategy: An Integrated Approach
The One Health concept is defined as an integrating, unifying approach that aims to sustainably balance and optimize the health of people, animals, and ecosystems. It recognizes the fundamental interconnectedness of the health of humans, domestic and wild animals, plants, and the broader environment, including all ecosystems.
Implementing the local One Health strategy requires an estimated US$ 45 million. A key aspect of this strategy is the envisaged role of NAC in advocating for the integration of an HIV-focused approach to strengthen regulations, promote responsible antimicrobial stewardship, and ensure access to necessary medications.
“NAC will be expected to integrate AMR education into existing HIV programs, train healthcare workers on rational prescribing practices, support targeted AMR research specifically within HIV patient populations, and champion necessary policy reforms and resource mobilization efforts,” Dr. Hodobo explained.
He further clarified the broad scope of the One Health approach: “The One Health approach that I mentioned is not just for HIV, but for other kinds of diseases that can affect people, ranging from foodborne infections to zoonotic diseases, which are transmissible from animals to humans, such as anthrax and rabies.”
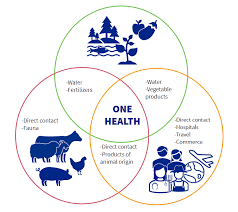
Dr. Hodobo also emphasized the critical need for greater awareness regarding the proper use of crop pesticides, including safe storage and disposal of chemical leftovers to prevent environmental contamination, which can indirectly impact human health.
Furthermore, the injudicious sale of antibiotics over-the-counter, inadequate sanitation practices, and the discharge of non-metabolized antibiotics or their residues through feces/manure and industrial effluents into the environment are significant factors exacerbating the problem of AMR.
The relationship between these contributing factors and the environmental spread of AMR is considerable and complex. Globally, infections caused by multidrug-resistant microbial pathogens lead to approximately 700,000 deaths annually. Alarmingly, if effective action is not taken, this annual death rate is projected to reach 10 million by 2050, exceeding the current mortality rate from cancer.
In recent years, antibiotic consumption in cattle and poultry has risen at an unprecedented rate across continents, a trend that is expected to accelerate by a further 67% by the year 2030 in rapidly industrializing and developing countries, which often face significant pollution challenges.
The growing global issue of AMR has also significantly increased the economic burden on healthcare systems worldwide.
In the context of HIV, drug resistance to opportunistic infections can also lead to the failure of antiretroviral therapy, underscoring the urgent need for developing nations like Zimbabwe to take proactive and comprehensive action to address the interconnected challenges of AMR and HIV.
